
CMS Hospital Value-Based Purchasing Program
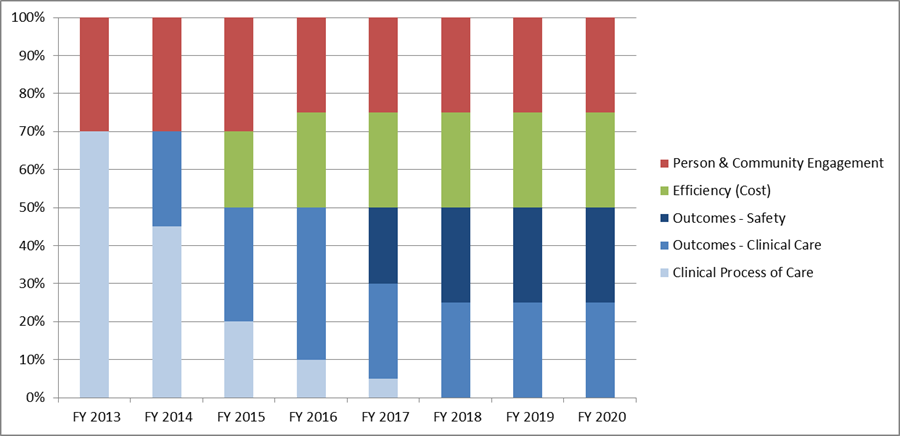
Relative weighting of quality measurement domains, FY 2013 – FY 2020
The Medicare Hospital Value-Based Purchasing (VBP) Program marked one of the first major steps made by the Centers for Medicare & Medicaid Services (CMS) in transitioning from a volume-based payment system to one in which providers are paid based on quality. Authorized by the Affordable Care Act of 2010, the Hospital VBP program provides financial incentives or penalties to hospitals based on their performance on a set of quality measures. As one of the longest-standing federal VBP programs, Hospital VBP has provided a model for the implementation and evolution of quality pay-for-performance programs for Medicare and more generally.
CMS has updated the Hospital VBP quality measure set and performance measurement method annually since the program’s inception in federal fiscal year 2013. When the program was first implemented, the measure set consisted entirely of clinical process of care measures and patient experience of care measures, with the former domain being weighted higher at 70% of a hospital’s total performance score. The initial focus on “process measures” was intended to ease providers into this new way of being paid for Medicare services, by focusing on measures more proximally within the control of providers.
In the second year of the program, the first clinical outcome measures were introduced. Clinical outcome measures are generally considered more meaningful than process measures as indicators of the quality of care provided, but performance on these measures is also subject to factors not directly within the control of a single provider, requiring a more holistic and coordinated approach to caring for a patient. As the program evolved, additional clinical outcome measures were introduced and represented an increasing portion of a hospital’s performance score (up to 50% as of FY 2018). The clinical process of care domain was phased out over this five-year period. The evolution toward the use of more meaningful outcome measures and reduced reliance on process measures later became one of the guiding principles of the Meaningful Measures initiative, which CMS launched in fall 2017.
Efficiency (cost of care) measures were introduced in the third year of the program. This enabled CMS to build upon a foundational focus on delivering high-quality care established in the first two years of the program before asking providers to take responsibility for reducing unnecessary medical spending. The patient experience of care domain (recently renamed Person and Community Engagement) has represented a relatively consistent portion of a hospital’s total performance score since the program’s inception, reflecting CMS’s continued prioritization of beneficiary engagement.