
[1] A few years ago, a custom-fabricated bioresorbable tracheal splint saved the life of an infant suffering from a collapsed bronchus due to severe tracheobronchomalacia.[2] The splint was implanted around the baby’s airway, expanding the bronchus and giving it a skeleton to assist with proper growth.[3] Twenty-one days later, the baby was off ventilator support and breathing normally.[4] The splint was the product of 3D printing (also known as additive manufacturing or “AM”). [5]
The U.S. Food and Drug Administration (“FDA”) and industry are currently grappling with how to address the unique issues related to 3D printing and its rapidly growing application in healthcare. While the implantable splint described above was for many people their first introduction to medical uses of 3D printing, other applications have included custom prosthetic limbs, hearing aids, drug formation,[6] and human kidney tissue, and recent reports predict that the global 3D printing medical/healthcare market will exceed $2.8 billion by 2022.[7]
In May 2016, FDA issued its much-anticipated draft guidance, “Technical Considerations for Additive Manufactured Devices,” providing its “initial thinking” on design, manufacturing, and device testing considerations related to AM devices.[8] This guidance is not intended to be a comprehensive road map for how FDA intends to regulate AM devices. Instead, FDA intends to use the “leap frog guidance”[9] as a mechanism to share FDA’s initial recommendations, which the Agency acknowledges may change as more information becomes available. Medical device manufacturers should carefully consider the impact of the draft FDA guidance on the potential uses of this technology as a supplement or alternative to traditionally manufactured devices. Hospitals, healthcare facilities, and clinics with the ability to make patient-matched devices should also carefully review the draft FDA guidance, since point-of-care manufacturing could raise regulatory issues and new requirements for these entities in the future. FDA is accepting comments on the draft guidance until August 8, 2016, and we expect there to be substantive comments filed from industry that ultimately will help shape FDA’s final guidance.
What Is Additive Manufacturing?
Additive manufacturing or 3D printing is the emerging process by which a three-dimensional object is made (or “printed”) by the repeated depositing of tiny layers of material—most often plastic or metal—on top of one another.[10] The process begins with the creation of a 3D blueprint with computer-aided design (“CAD”) software, continues to the printing stage, and after anywhere from a few minutes to a few days (depending on the size and complexity of the design), concludes with the creation of an intricate object.[11] Importantly, the process is capable of producing designs often far more complex and detailed than would be possible with other, more traditionally used approaches.
AM holds potential advantages for many industries, allowing designers to create a nearly limitless array of shapes that can be altered and varied without much difficulty. The manufacturing potential that 3D printing holds is perhaps nowhere more promising than in the medical field. In particular, AM has “the advantage of facilitating the creation of anatomically-matched devices and surgical instrumentation by using a patient’s own medical imaging.”[12] In other words, 3D printing makes the creation of medical devices designed for a specific patient easier, meaning that one-size-fits-all medical devices eventually could be a thing of the past.
How Has FDA Regulated Additive Manufactured Devices?
As of December 2015, FDA has cleared more than 85 medical devices constructed either in part or entirely through the use of 3D printing.[13] The types of devices that have been cleared are various, including orthopedic and cranial implants, tools used in surgery, dental structures such as crowns, and external prosthetics.[14]
Currently, it appears that FDA is viewing devices manufactured through the use of 3D printing under its existing device premarket regulatory regime. In other words, an AM device’s regulatory classification continues to be determined by the regulatory classification of the same non-AM device.[15] However, at some point FDA may conclude that the manufacturing process and/or design changes related to AM manufacturing raise new questions of safety and effectiveness. If that is the case, AM manufactured devices may be considered “new” Class III devices requiring the submission and approval of a premarket approval application (“PMA”) or a “de novo” submission. It will also be interesting to see whether the definition of “manufacture” and “manufacturer” will evolve. At this time, these terms are defined broadly and include the design, manufacture, fabrication, assembly, or processing of a finished device.[16] If left as is, non-traditional entities, such as healthcare providers and suppliers, which use 3D printers to customize devices, could be regulated as manufacturers and therefore be required to comply with new and significant regulatory requirements.
Draft Guidance: Technical Considerations for Additive Manufactured Devices
In May 2016, FDA issued its first guidance on AM, “Draft Guidance: Technical Considerations for Additive Manufactured Devices.”[17] FDA indicates that AM devices will “generally follow the same regulatory requirements as the classification and/or regulation to which a non-AM device of the same type is subject to” and that only in “rare cases” will AM raise “different questions of safety and/or effectiveness.”[18] The draft guidance highlights issues specific to AM devices for industry to also consider through the phases of development, production process, process validation, and final finished device testing and in compiling premarket submissions for FDA review.[19] FDA provides the following flow chart to illustrate the overall AM process.[20]
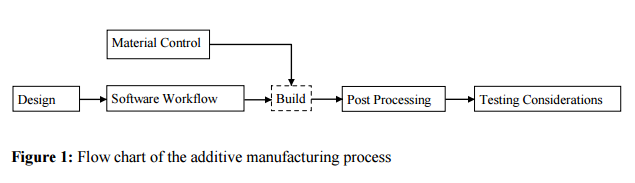
The extensive and detailed recommendations provided by the guidance apply to devices that include at least one AM step.[21] The draft guidance is broadly organized into two main topics: (1) Design and manufacturing considerations and (2) Device testing considerations. We address each topic below in turn.
Design and Manufacturing Considerations
This section of the guidance addresses technical considerations to fulfill the Quality System (“QS”) requirements.[22] Recognizing that different AM technologies and processing step combinations exist, FDA emphasizes the importance of clearly identifying each critical step in the printing/manufacturing process.[23] FDA suggests using a production flow diagram augmented by a description of the process and identification of process parameters and output specifications.[24] Risks and mitigations should be identified and documented for each step of the manufacturing process.[25]
Below are some of the key design and manufacturing considerations:
-
Device Design
-
For standard-sized devices (i.e., devices offered in pre-established discrete sizes), manufacturers should document dimensional specifications for the final device or component and manufacturing tolerances of the machine to confirm that the device or component can be “reliably built” with the “chosen additive technology.”[26]
-
For patient-matched devices[27] (i.e., device based on a standard-sized template model matched to a patient’s anatomy), clinical staff, manufacturers, or a third party can modify these designs in response to clinical inputs. Accordingly, to avoid adverse consequences, manufacturers should clearly identify clinically relevant design parameters, including the minimum and maximum for these parameters and which can be modified for patient-matching.[28] If medical imaging data is used to manufacture the device, manufacturers should consider issues including image quality, rigidity of anatomic structures being imaged, and potential constraints in light of necessary manufacture time and changes in anatomy.[29] Furthermore, any software or procedure used to modify the device design based on clinical input should include “internal checks that prevent the user from exceeding the pre-established device specifications documented in the device master record.”[30]
-
Software Workflow
-
All file conversion steps should be tested with simulated worst-case scenarios to ensure expected performance.[31]
-
Manufacturers should consider the following preparatory processes for after the digital device design is finalized, but before the device can be additively manufactured: (1) build volume placement, (2) addition of support material, (3) slicing model with focus on choice of layer thickness, and (4) determining and creating build paths (i.e., the path traced by the energy or material delivery system, such as the laser or extruder) and fill density. All decisions related to these preparatory processes should be documented.[32]
-
Manufacturers should consider the variability of machine parameters and environmental conditions for the specific AM technology and machine model. Manufacturers should maintain proper calibration and perform preventative maintenance.[33]
-
Material Controls
-
Manufacturers should:
-
Document the following information for each starting material, processing aid, additive, and cross-linker used: (1) identity of the material or chemical by common name, chemical name, trade names, and Chemical Abstracts Service (CAS) number, (2) material supplier, and (3) incoming material specifications and material certificates of analysis (“COAs”), with the test methods used for the COAs.[34] Specifications for incoming materials and test methods should be based on the AM technology used.[35]
-
Document any change in material specification, including the effect on the build process and the final device.[36]
-
Describe any material recycling process and evidence that material recycling does not adversely affect the final device.[37]
-
Post-Processing
-
Manufacturers should document all post-processing steps (i.e., manufacturing steps occurring after the printing process). Documentation should include discussion of the effects of post-processing on materials used and on the final device as well as identifying potentially detrimental effects of post-processing and mitigations implemented.[38]
-
Process Validation and Acceptance Activities
-
Manufacturers should:
-
Perform and document process validation methods and data to “ensure and maintain quality for all devices and components built in a single build cycle, between build cycles, and between machines,” including software.[39] Methods include in-process monitoring of parameters, manual or automated visual inspection with defined acceptance criteria, non-destructive evaluation, and test coupon evaluation.[40]
-
Revalidate changes to manufacturing process or process deviations, including change or update of build preparation software, changes in material or material handling, and changes to the software workflow.[41]
-
Perform acceptance activities to ensure repeatability and consistency within a build cycle and across lots.[42] Some nondestructive evaluation techniques to consider when verifying geometry, microstructure, and performance characteristics include ultrasound, computed tomography, and X-ray.[43]
-
Quality Data
-
Manufacturers should analyze sources of quality data to identify existing and potential causes of nonconforming product or other quality problems.[44]
Device Testing Considerations (for Premarket Submissions)
This section of the guidance outlines the type of information FDA recommends manufacturers include in a premarket submission for an AM device. All of the requested information is not necessarily applicable to a single device. Furthermore, as FDA explains, “if the type of characterization or performance testing outlined [in the guidance] is needed for a device made using non-AM techniques, the information should be provided for an AM device of the same device type.”[45]
We highlight below some of the key elements for a premarket submission for an AM device:
-
Device Description: This may include an AM process flow chart, technical drawings, and information regarding device dimension range, design variations, critical dimensions or features intended to be patient-matched, and type of AM technology used.[46]
-
Mechanical / Performance Testing: Such testing will generally be the same as that for a non-AM device.[47] Manufacturers also should consider the build orientation and location within the build space.
-
Dimensional Measurements: Specify dimensional tolerances and perform dimensional measurements for each AM component.[48] Manufacturers should make dimensional measurements on samples from multiple build cycles or use process validation information to demonstrate negligible variability between build cycles.
-
Material Characterization:Identify all materials involved in device manufacturing, all expected material chemistry changes, all material properties affecting interlayer bonding, and specific physical material properties based on the underlying type of material (e.g., metal, ceramic, polymer, or absorbable material). [49] Additional testing may be necessary depending on the type of material.
-
Cleaning and Sterilization:The complex geometries of AM devices present significant cleaning and sterilization issues.[50] Accordingly, cleaning and sterilization process validation should test the complex geometries under worst case scenario conditions and account for adequate removal of residual manufacturing materials. The premarket submission should also indicate that the device is cleaned of manufacturing materials before being provided to the end user. Manufacturers should consider sterilizing the device prior to providing it to the end user.
-
Labeling: Additional labeling information should be included for AM devices that are patient-matched, since clinical staff, device manufacturers, or third parties might modify the device design.[51] The patient-matched device should be marked or have accompanying physician labeling to identify the patient identifiers, details identifying use/anatomical location, and final design iteration or version used to produce the device. Labeling should also include an expiration date based on the patient-imaging date or design-finalization date and a precaution that the patient should be surveyed for potential anatomical changes prior to procedure.
Conclusion
Although FDA’s draft guidance provides an initial starting point for AM devices and the regulation of the emerging technology, many unknowns still remain. Accordingly, it remains prudent for manufacturers to use FDA’s pre-submission process to obtain more detailed feedback regarding their specific AM device or process.
To better understand the technology and the effect of different printing techniques and processes on the safety, effectiveness, quality, and performance of FDA-regulated products, FDA’s Office of Science and Engineering is investigating how the technology may affect medical device manufacturing in the future. Its projects include developing and adapting computer-modeling methods to determine the effect of design changes on safety and performance of devices and studying “how different printing techniques and processes affect the strength and durability of the materials used in medical devices.”[52] To the extent FDA concludes there may be a significant impact on safety or effectiveness, FDA may impose more rigorous controls and/or requirements on devices manufactured by AM.
In the meantime, the 3D printing industry continues to grow at a rapid pace. Developing areas of future interest include personalized medicine through point-of-care manufacturing and bioprinting. With the greater availability of 3D printers and the ability to print patient-matched devices on demand, healthcare facilities, hospitals, clinics, academic centers, and practitioner offices are increasingly “manufacturing” devices on-site. It is unclear whether and how FDA will regulate such entities. In its draft guidance, FDA states simply that “[p]oint-of-care device manufacturing may raise additional technical concerns,” but did not provide any further guidance.[53] Likewise, FDA does not address AM biological, cellular, or tissue-based products – or “bioprinting” – in its draft guidance except to direct such questions to the Center for Biologics Evaluation and Research. Bioprinting creates tissue-like structures through 3D printing of cells, utilizing the layer-by-layer fabrication method to print tissues and organs.
AM provides the health industry with new, exciting, and potentially life-changing opportunities for healthcare advances. Medical device manufacturers not yet working in the AM space should consider whether and how the technology could apply to its devices, and non-traditional stakeholders, such as healthcare providers and suppliers, should carefully consider how FDA’s regulatory framework may apply to them. Accordingly, we encourage a close review of FDA’s draft guidance and its future statements on 3D printed devices and manufacturing. We will continue to monitor FDA developments in this evolving area and associated challenges in the coverage, reimbursement, and products liability areas.
Notes:
[1] We thank our K&L Gates summer associate, Eli Schooley, for his assistance with this Alert.
[6] In August 2015, FDA approved the first 3D printed drug product, Aprecia Pharmaceuticals’ epilepsy drug, SPRITAM (levetiracetam). According to Aprecia, its 3D printing technology allowed the company to produce a porous formulation that “rapidly disintegrates with a sip of liquid.” See Aprecia Pharmaceuticals Press Release, “FDA Approves the First 3D Printed Drug Product” (Aug. 3, 2015), available at: https://aprecia.com/pdf/2015_08_03_Spritam_FDA_Approval_Press_Release.pdf.
[8] FDA 3D Printing Draft Guidance.
[9] A “leap frog guidance” is a newer mechanism for FDA to “share initial thoughts regarding emerging technologies that are likely to be of public health importance early in product development.” FDA 3D Printing Draft Guidance at 2.
[12] FDA 3D Printing Draft Guidance at 3.
[16] 21 CFR 803.3, 807.3, 820.3(o).
[17] In October 2014, FDA convened a public workshop with medical device manufacturers, AM companies, and academia to discuss technical considerations for AM medical devices. FDA 3D Printing Draft Guidance at 3. The workshop focused on the following themes: (1) materials, (2) design, printing, and post-printing validation, (3) printing characteristics and parameters, (4) physical and mechanical assessment of final device,; and (5) biological considerations of final devices, including cleaning, sterility, and biocompatibility. Id. The feedback from the workshop served as the basis of the draft guidance. Id. at 4.
[22] The guidance document is not intended to comprehensively address all QSR requirements. See id. at 6. Manufacturers should refer to 21 CFR Part 820 and any specific device type regulations to determine what QS requirements apply. Id.
[27]Although often referred to as “customized” devices, these devices are not “custom devices” meeting the Federal Food, Drug, and Cosmetic Act’s custom device exemption requirements unless they otherwise comply with all of the criteria of FDCA 520(b). Id.
[40] Id. at 17. Test coupons are representative test samples of a device or component and can be used for process validation, to identify worst-case condition in the manufacturing process, and confirm that the components or devices built in the same build cycle will meet specifications if the test coupons meet the specifications. Id. at 18.
[52] Steven K. Pollack and James Coburn, FDA Goes 3-D (FDA Voice Aug. 15, 2013).
[53] FDA 3D Printing Draft Guidance at 2.