 Medical specialists and researchers have taken a big step in recognizing that how they diagnose black patients with kidney disease may be racially biased and harmful to a group that already and disproportionately suffers the illness’s harms.
Medical specialists and researchers have taken a big step in recognizing that how they diagnose black patients with kidney disease may be racially biased and harmful to a group that already and disproportionately suffers the illness’s harms.
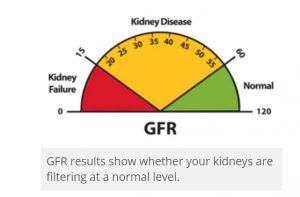
Doctors now should jettison race-based adjustments in equations used in a crucial and fundamental test to assess kidney function, according to studies and editorials published in the New England Journal of Medicine, the American Journal of Kidney Diseases, and the Journal of the American Society of Nephrology.
As the New York Times reported, this step will “affect hundreds of millions of kidney function tests performed yearly in hospitals and outpatient settings, both for acutely ill patients and as part of routine screening blood tests. By one estimate, one million Black Americans might be treated earlier for kidney disease if the diagnostic equation were not adjusted for race.”
The newspaper reported this of the race-based diagnostic calculations that affected black patients:
“The [earlier] adjustment may make black patients seem less ill than they really are, according to many experts. Instead, doctors should rely on a race-neutral method for diagnosing and managing kidney disease, concluded a report from the National Kidney Foundation and the American Society of Nephrology.”
The medical establishment had compelling reasons to reexamine its testing bias, especially when confronting the terrible toll that kidney disease afflicts on people and communities of color, the New York Times reported:
“Black and Hispanic Americans have long suffered from high rates of conditions such as diabetes, high blood pressure, and obesity, which can exacerbate a bout of Covid. These factors can also increase the risk of developing kidney disease. The racial disparities in kidney disease are stark and well documented. black Americans are more than three times as likely as white Americans to experience kidney failure and require dialysis or a kidney transplant. Though black Americans make up only 13% of the population, they represent 35% of Americans with kidney failure. More than 90,000 Americans are on a waiting list for a kidney; nearly one-third are black, about as many as those who are white.
“People of color and low-income Americans are less likely to receive good care when the warning signs first appear and chronic kidney disease could be prevented. They are more likely to progress to kidney failure and to require dialysis, and less likely to be cared for by a kidney specialist before getting to that stage, according to a report by the Centers for Medicare and Medicaid Services. Black Americans also wait longer for an organ, and are less likely to have a kidney donated by a friend or relative, for a variety of complex reasons.”
Dr. Nwamaka Denise Eneanya, a nephrologist at the University of Pennsylvania and a member of the task force that recommended the race-free diagnostic change, told the newspaper this about reasons why it was needed:
“’This new recommendation will ensure that racial biases are not introduced to clinical care, so someone will no longer be judged based on their race and have their skin color dictate what kidney care they receive’ … Her work suggests that current measures used to assess kidney function may underestimate the severity of illness in lack patients, delaying referrals to specialists and making them less likely to be placed on waiting lists for a kidney transplant. ‘Black individuals are inadvertently harmed because they are seen as not sick enough,’ Dr. Eneanya said.”
The newspaper reported that concerns have risen among clinicians about racial discrimination in tools doctors use to diagnose and treat a variety of conditions “from bone density and kidney stones to cancer and pulmonary function tests.”
Many more tests these days are run at large-scale by machines. Experts, attempting to adjust for human discrepancies, may inject casual observations with resulting racial bias into algorithms that employ math or logic to help doctors process big quantities of data. As a study published in August in the New England Journal of Medicine reported, the kidney function test in part measures levels in the blood of creatinine, a waste product in muscle metabolism. Without understanding exactly why black patients may show higher levels of this substance, the kidney function test includes an algorithm that adjusts for this and skews results:
“These algorithms result in higher reported eGFR values (which suggest better kidney function) for anyone identified as black. The algorithm developers justified these outcomes with evidence of higher average serum creatinine concentrations among black people than among white people. Explanations that have been given for this finding include the notion that black people release more creatinine into their blood at baseline, in part because they are reportedly more muscular. Analyses have cast doubt on this claim, but the ‘race-corrected’ eGFR remains the standard.”
Follow-up research must be done to see if the relatively simple to accomplish algorithm correction eliminates, as experts argue it will, a major bit of racial discrimination in medicine, resulting in improved diagnosis and care for black patients. Here’s hoping.
In my practice, I see not only the harms that patients suffer while seeking medical services, but also their struggles to access and afford safe, efficient, and excellent medical care — and to understand and control what’s happening to them and their loved ones in a daunting system. Health care has become an ordeal for patients due to its skyrocketing complexity, uncertainty, and cost for treatments and prescription medications, too many of which turn out to be dangerous drugs.
It is unacceptable that, for patients of color, contemporary medicine imposes racially discriminatory hurdles to the safety and quality of their care. While doctors, medical scientists, hospitals, insurers, and other parties in the U.S. health care system pursue higher profits and greater efficiencies, especially with computerization and mechanization of processes, they must exercise great care to safeguard patients from malicious gremlins in their “innovations.” It is abhorrent to know that big brains might be building racism, sexism, ageism, or other terrible biases into machines.
We have a lot of work to do to ensure that health care is a right, not a privilege in the wealthiest nation in the world. And that it is accessible, affordable, safe, efficient, and excellent — for all humans, without inappropriate racial discrimination.